
His general practitioner encouraged him to complete an advance care directive. He does not want to become someone that no one recognizes and he has grieved that he is unlikely to see his children marry. He had seen his mother suffer with dementia and have a poor end of life. He told Lucy that he was distressed to think the future involved him not recognizing his family and friends. Prior to this decline, Andrew and Lucy discussed his future on many occasions.

His wife Lucy is his support person and will be his substitute decision-maker (when he is deemed to have lost decision-making capacity). In the last two years, there has been a rapid decline in Andrew’s functional status. He was diagnosed with early onset dementia three years ago. Andrew: an example scenarioĪndrew is a retired 64-year-old who is married and has young adult children. Let's consider each of these in relation to the scenario below. promote congruence between individuals and substitute decision-makers.promote patient autonomy through a case-based approach to ethical decisions.Healthcare professionals and settings can take four actions to promote better decision-making in situations where ethical considerations arise. It also involves important questions of whether the individual still retains some decision-making capacity, albeit diminished. This often involves questions of whether an advance care directive should or should not be upheld given current competing factors. This means the individual's past desires previously expressed in an advance care directive versus their current interests. A substitute decision-maker makes decisions for someone who has no decision-making capacity.) Precedent versus contemporary autonomyĪ common theme within ethical debate regarding advance care planning is precedent versus contemporary autonomy of the individual. (A support person is someone who helps a person with reduced capacity make decisions. Individuals who are able to make decisions with the support of healthcare professionals or a support person should be given the opportunity for them to maintain their autonomy whenever possible. The existence of an advance care directive should not preclude or replace the individual’s right to make decisions whilst they are able to do so. Individuals should be engaged in current decisions about their care to the greatest extent possible. Enacting advance care directivesĪdvance care directives should be enacted only when an individual cannot make decisions for themselves.
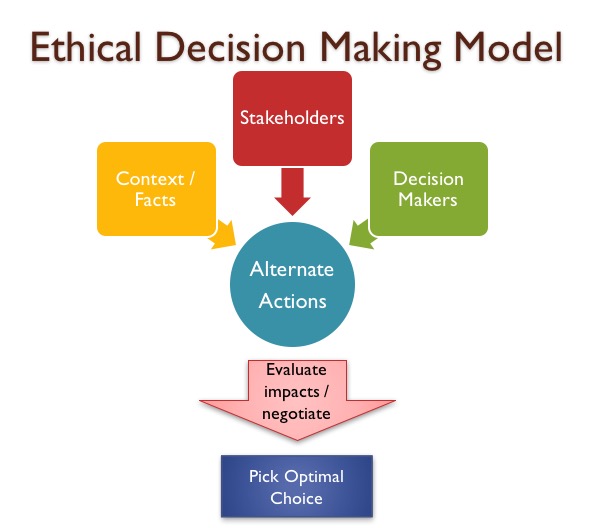
Rarely will the law and an advance care directive provide sufficient directions or preferences for decision-making under all circumstances. Medical treatment decision-making on a case basis requires ethical considerations. The Australian advance care planning legal framework may be helpful but the law needs interpreting and applying to specific cases. Implementing legal frameworks for advance care planning and end-of-life care is problematic because ethical and moral issues are relevant factors in medical treatment decision-making. Medical decision-making towards the end of life can be difficult for everyone concerned and involves complex ethical considerations and situations where there isn't one 'right' way forward.Įthical reasoning is a significant component of advance care planning which affects the actions of the individual concerned as well as their family, friends, carers and medical team.


 0 kommentar(er)
0 kommentar(er)
